The crown of my head begins to tingle. It spreads down through the rest of my head, into my face and my neck. It’s like that warm electrical charge you feel when you’ve sat in the sun for too long, except it doesn’t fade away as my body gets cooler. It just keeps tingling.
Then my chest tightens — smack dab in the center. Always in the center. Initially, it feels like indigestion when something you eat is taking an extra-long time moving through your esophagus into your stomach — but it doesn’t ever move. It progresses from being tight and uncomfortable into a squeeze that makes me wonder if I am having a heart attack. I am out of breath. I am sweaty. And I wonder if I should call 9-1-1.
That is what it feels like when I have a full blown anxiety attack.
My anxiety attacks are almost always preceded by a series of anxiety episodes.
During the episodes, I am fidgety and forgetful, and I cannot focus. I am easily irritated by normal inconveniences. I cry uncontrollably when too many inconveniences happen to me at the same time. And, I am very, very tired, no matter how much sleep or rest I get.
I am self-aware enough and comfortable enough now with my disease that 90% of the time, I can catch myself in the first day or two of an episode and manage my symptoms before a full attack begins.
I do a lot of breathing exercises. I meditate. I journal. I drink all kinds of teas. I do EFT Tapping exercises. I communicate daily with my therapist. I take CBD edibles alongside my regular anxiety medication dosage. Even with all these interventions, it usually takes me three or four days to get back to feeling normal.
I do most of these things even when I’m not having an episode because they help me feel calm and capable. But sometimes, despite my best efforts, the episodes and/or the full-blown attacks just hit me out of nowhere and there’s nothing I can do but let them pass … in those moments, I resent my brain and body for having this disease.
Like many people with mental health issues, I mask and downplay my challenges at work. I do not want my bosses, colleagues, or the team that I lead to look at me differently. Share on XLike many people with mental health issues, I mask and downplay my challenges at work. I do not want my bosses, colleagues, or the team that I lead to look at me differently. I don’t want them to avoid telling me things that may be stressful for fear of causing an attack, or for them to assume that I am having an episode anytime I have a bad day. I don’t want to be judged or stigmatized. So, I don’t talk about it unless I absolutely have to — and when I do, it is with very select individuals and in the strictest of confidence.
Until now.
Once they read this, they’ll all know, and it is likely things will change. And I am OK with that.
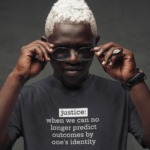
Stopping the stigma, particularly around Black mental health, requires people to talk openly and specifically about our mental health challenges as well as the help we are getting to manage and overcome these diseases. This must include talking about being in therapy and taking prescription medications. This must also include talking about the difficult and traumatic experiences which caused the breakdowns that triggered our conditions. We must speak our full truth.
Stopping the stigma, particularly around Black mental health, requires people to talk openly and specifically about our mental health challenges as well as the help we are getting to manage and overcome these diseases. Share on XIn the workplace, it can be difficult as a manager to know what to do for someone who reveals to you that they have a mental health disorder. No matter the person’s race or gender identity, the stigma associated with mental health disorders affects everyone. As managers and leaders, we are often unprepared for how to navigate it.
Here are three tips based on my experience as someone living with anxiety disorder and as someone who is an expert on people-management techniques:
- Let them lead. People who are open about their mental health challenges and disorders are often actively managing them, so they know what they need to cope when a serious episode flares up. Do not assume their needs or desires based on your experiences with others or what you read on the internet (doing this is also in opposition to Americans with Disabilities Act guidance as well). Ask them and let them make their requests for support to you.
- Keep their confidence. Don’t go sharing with others about their diagnosis. The only other person/group you will want to notify is your Human Resources (HR) department so they can help you navigate potential legal issues, accommodation or leave requests, etc. Otherwise, the information should stay between you and the individual.
- Give real support. Once someone has revealed their diagnosis and shared how you can support them, and you’ve consulted with HR, you should then educate yourself on the disorder and, based on what the person has said their needs are, figure out ways to support them. This may be time off or remote work or a more flexible schedule. This may be setting task alerts with them in an online system to help them complete their work by the deadlines. This may be reassigning all or part of project to allow them time to recover from an episode. This may be moving their seating closer to a door, window or bathroom to help limit some of their triggers … There are no one-size fits all approaches to mental health support — but being compassionate, committed and creative in your approach is always a great place to start.
The National Institute of Mental Health Disorders estimated in 2019 that 26% of American adults will suffer from a diagnosable mental health disorder in a given year. That is slightly more than 1 in 4 people. So, the chances that we will encounter someone in our workplaces and on our work teams who struggles with a mental health disorder are high.
As leaders committed to creating inclusive and psychologically safe environments, we have to be prepared for what we will do when someone reveals a diagnosis to us. Because what we don’t want to do is make a person feel judged, rejected or stigmatized for a disease they did not choose as part of their existence and have little control to change. That would be the opposite of living and working inclusively.
This is my moment of full truth surrounding my anxious mind. No more downplaying. No more masking. I hope it inspires someone with a mental health disorder to speak their truth. And I hope it encourages someone managing an employee with a mental health disorder to do better.