Sixteen years ago, I delivered my son by emergency cesarean section. I had gone to the maternity ward three times in 36 hours. When they were preparing me to be discharged during the second visit, I was beginning to question myself. I knew something didn’t seem right. My normal active baby was going for hours not moving, and I was leaking fluid from what I could tell. The doctors checked me out the first and second time. They told me everything was fine. I was to go home and wait to go in labor.
I got dressed and was sitting on the edge of the bed during my second visit, when the nurse came in to go over my discharge paperwork. Luckily for my son and me, she went a little off-script toward the end. She told me that I had been carrying my baby for nine months. She assured me that if I felt something was wrong to come back. Do not question it. Come in. I returned that third time. At that point, they informed me that I had too little fluid and the contractions were restricting my son’s heart from pumping properly. I was rushed into surgery. My son was born. He spent an extra couple of days in the hospital due to jaundice after I was discharged.
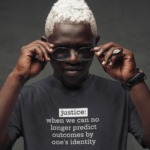
I tell this story to give a face to the idea of medical discrimination. I honestly can’t say that the doctors didn’t take me seriously because I was a woman or a Black woman. But I can say that the medical professionals didn’t believe me. I can say that had that nurse not said what she said, I may not have returned. My son could have died. I could’ve died. As bizarre as it sounds, I have had Black women say that medical professionals told them that Black women couldn’t feel pain. Why wouldn’t we be able to feel pain as human beings?
I tell this story to give a face to the idea of medical discrimination. The medical professionals didn't believe me. My son could have died. I could've died. Share on XThe United States maternal mortality rate is 17 per 100,000 births. For Black women, it’s 43 per 100,000 births. What is happening in our medical facilities that Black women are dying at more than twice the general population’s rate? That’s a complex question to answer and certainly not what I am prepared to attack in this article.
The U.S. maternal mortality rate is 17 per 100,000 births. For Black women, it's 43 per 100,000 births. What is happening in medical facilities that Black women are dying at more than twice the general population's rate? Share on XInstead, I want readers to consider the implications of medical discrimination in the context of us emerging from a global pandemic. COVID-19 has revealed a lot of things. It most certainly revealed that Black and Hispanic people had poor health outcomes through many social determinants of health. This is a consistent trend across almost all disease states and viruses: Black people are twice as likely to be diagnosed with Multiple Myeloma, an incurable blood cancer, then their white counterparts; twice as likely to experience a stroke; more likely to die of cancer and asthma, and more likely to be diagnosed with diabetes and associated complications.
Even when People of Color have the same levels of education, finances and insurance, they have less positive health outcomes than their white counterparts.
A year ago, we watched a white man murder a Black man by kneeling on his neck. We called for police reform. We watched this while being locked down. We couldn’t turn away.
As we begin to emerge from this global pandemic, we can’t look away. We have to continue to understand and dismantle the barriers toward equitable healthcare delivery. We must reform all institutions that do not provide a level playing field for all communities. We cannot look away any longer.
As we emerge from this pandemic, we have to continue to understand and dismantle the barriers toward equitable healthcare delivery. We must reform institutions that don't provide a level playing field for all communities. Share on X




![The Buzz: The [Black] Dolls Are in Town](https://theinclusionsolution.me/wp-content/uploads/2024/04/Young-Black-girl-with-Black-baby-doll-440x264.jpg)