Content warning: This post contains discussion of and themes surrounding anti-fat bias and body shaming by medical professionals.
My experience with medical fat phobia
Have you hesitated going to the doctor because you’re worried you won’t be taken seriously? You dread sitting in a doctor’s office because you never know if they’ll shame you for the way you look … but you’re dealing with health issues and don’t know what else to do.
I’ve been there, too.
After months of concerning GI symptoms, I was finally seeing a specialist to figure out what was going on. I was looking forward to getting answers. And then I met the doctor.
No greeting or introduction. No eye contact. Without even glancing at me, his first words were, “Do you know your BMI?” He asked what I do for a living and when I told him I’m a nurse, he acted completely shocked. He asked how I could let this happen. I’m a nurse and should “know better.” I was too embarrassed to answer.
He didn’t ask about diet.
Didn’t ask how much physical activity I was getting.
Didn’t ask a single question about healthy behaviors.
With a BMI that landed me in the category of “obese” he believed he had all the information he needed. He lectured me about how to lose weight and dismissed all my concerns.
I came in with symptoms of serious health conditions. If I was in a smaller body, I’m confident I would have gotten immediate diagnostic testing. Instead I was told to “cut out snacks and see what happens in a few months.” I know my care would have been better if my body looked different.
I came in with symptoms of serious health conditions. If I was in a smaller body, I’m confident I would have gotten immediate diagnostic testing. Instead I was told to 'cut out snacks and see what happens.' Click To TweetMy experience is all too common.
It led me down a rabbit hole of trying to find providers who would treat me like a human being rather than a number on the scale. What I learned along the way changed my perspective on weight. It sent me on a journey toward self-love and fat liberation.
I learned that weight isn’t as directly related to health as we’re told. I’m working to drop words like “overweight” and “obese” from my vocabulary. They medicalize weight and imply that there’s a “correct” amount to weigh and anything over that is bad. I’m embracing the word “fat” as an adjective and nothing more.
Weight isn't as directly related to health as we're told. I’m working to drop words like 'overweight' and 'obese' from my vocabulary. They medicalize weight and imply that there’s a 'correct' amount to weigh. Click To TweetI want to spread the word about the complicated way weight impacts health. It’s not as cut and dry as we’ve always been taught. Critically: Anti-fat bias in healthcare and beyond is harming our health.
Anti-fat bias and weight stigma impact patient care
Studies show providers spend less time with large patients and show a strong anti-fat bias toward them.¹ Often patients in large bodies are told to lose weight before any further testing will be done. This causes considerable delays in the diagnosis and treatment of some serious conditions.
Studies show providers spend less time with large patients and show a strong anti-fat bias. Patients in large bodies are told to lose weight before any further testing will be done. This causes delays in diagnosis and treatment. Click To TweetAre these doctors at least helping patients get healthier by recommending weight loss? Anyone with a high BMI should strive to lose weight to be their healthiest, right? Well … no. Not really.
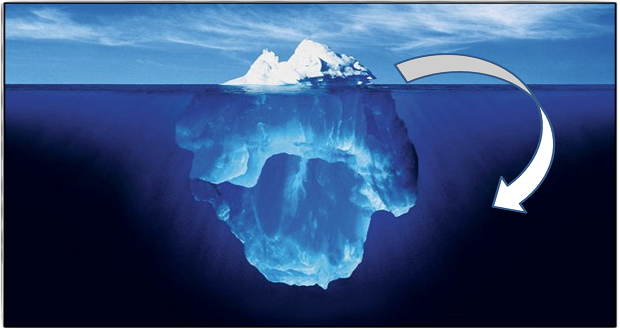
It’s so ingrained in our society that thin is healthy and fat is unhealthy, it may initially feel wild to consider this may not be true. Many studies use the phrase “obesity paradox” to explain findings that don’t show higher weight being harmful to health.
Researcher Katherine Flegal says, “You can report the same findings about obesity 100 times, and it can be called ‘unexpected’ every single time. It’s like, well, at what point would you change your mind and say this might be the expected result?”²
Putting emphasis on weight rather than behaviors misses the mark
Oftentimes, patients are told to lose weight without any guidance on how to safely do that. Some lose weight in unhealthy ways but are still congratulated by healthcare providers.
When the emphasis is on weight loss rather than establishing healthy habits, people are more likely to abandon them if they aren’t losing weight. Healthy behaviors like exercise, eating fruits and vegetables, and getting enough sleep are better indicators of health than weight.
When the emphasis is on weight loss rather than habits, people are more likely to abandon them if they don't weight. Behaviors like exercise and eating fruits and vegetables are better indicators of health than weight. Click To TweetHeavy people have a higher chance of cardiovascular disease than “healthy weight” individuals. Yet, anywhere from one-third to three-fourths of “obese” people are cardiovascularly healthy, and one-fourth of “normal” weight individuals fall into the category of “lean unhealthy.”³
Thin individuals who don’t practice healthy behaviors are twice as likely to develop Type 2 Diabetes as large individuals who do.³ Teaching that weight is the best predictor of health is a disservice to people of all sizes.
Previous harmful experiences prompt fat patients to avoid doctors
A lot of people in large bodies avoid going to the doctor until it’s an emergency. Challenges faced at earlier medical appointments make people not want to try again. Whether they felt judged for their size or faced a blood pressure cuff that didn’t fit, these experiences are harmful.
Women are especially likely to delay preventative care because of previous bad experiences. In America, large women are more likely to die of breast or cervical cancer than slender women. This is in part due to reluctance to get regular health screenings.⁴
Weight stigma is linked to a shorter life expectancy
Healthcare professionals, friends, family, and even strangers feel they can shame or blame a person in a larger body for “their own good.” This idea that anyone can look at another person and know their health status is untrue and harmful.
Healthcare professionals, friends, family, and even strangers feel they can shame a person in a larger body for 'their own good.' This idea that anyone can look at another person and know their health status is untrue and harmful. Click To TweetUp to 40 percent of people classified as “obese” report feeling stigmatized every day. Experiencing discrimination causes stress which is associated with lower life expectancy compared to similar weight individuals who don’t feel frequent stigmatization.⁵
Opportunity for a more inclusive society
Eliminating fat-phobia and anti-fat bias in healthcare would go a long way in changing the narrative around weight. Loved ones and strangers alike feel the right to shame people in large bodies under the guise of caring for their health. Removing weight from the conversation will create a more inclusive world for all of us.
Sound off in the comments — what are your thoughts on uncoupling weight from discussions about health?
References